Cuboid Syndrome & Recurrent Ankle Sprain
SIDE VIEW OF THE LATERAL (OUTSIDE) SIDE OF THE RIGHT FOOT. THIS IS A FLEXIBLE PLASTIC ANATOMICAL MODEL. I PLACED A LOOSE CUBOID BONE JUST BELOW THE CUBOID IN THE FOOT AND ANKLE MODEL. NOTE THE VERY LARGE CALCANEAL BONE TO THE LEFT (BEHIND). I TRULY ADVOCATE THE EVALUATION AND TREATMENT OF ANY MOTION RESTRICTION OF THE SUBTALAR JOINT (CUBOID AND TALUS) IN THE PRESENCE OF CUBOID SYNDROME. THE LITERATURE IGNORES THIS RELEVANT CONCEPT.
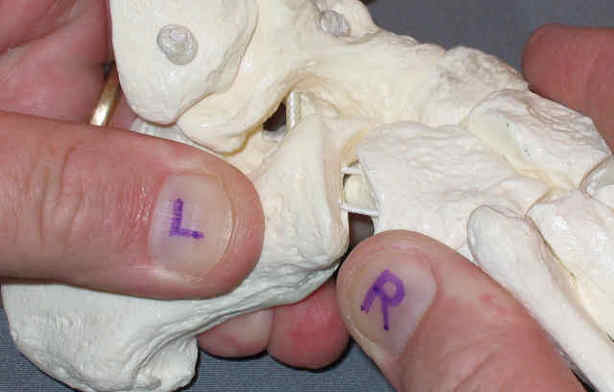
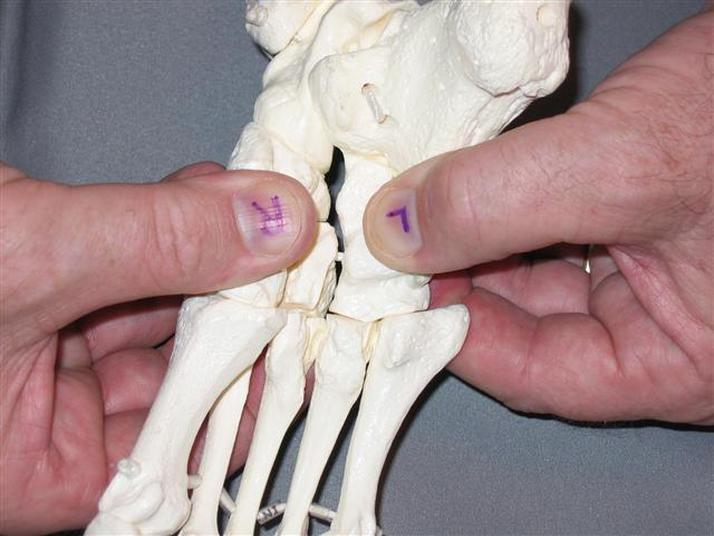
This images shows the undersurface of the foot. Thumb with an upside down "L" is the Cuboid. It articulates with the 4th and 5th Metatarsals below and with the Medial Cunieform and Navicular. Note that these joint are much more planar. This flatness indicates that the primary motion with an up and down glide.
I want to make a very important point. The cuboid is profoundly influenced by the calcaneus. The calcaneus is much larger and has a much greater mechanical advantage on the cuboid, inducing rotation. If you look at the joint formed by cuboid and calcaneus, you will see that it allows rotation, which participates in both functional pronation and functional supination. If a cuboid is chronically symptomatic, and it requires repeat treatment, look at the calcaneus. Work on restoring calcaneal eversion/valgus. The secret? Does anyone know this? One can easily restore normal calcalneal valgus/eversion and by mobilizing the sub talar joint; the joint where the calcaneus and the bottom of the talus connect. However, I do address all other major motions of the foot and ankle which are described below (See Major Motions of the Foot and Ankle in the section titled: Cuboid Syndrome). With client lying prone (face down), or kneeling on a treatment table, with feet off the edge. Clasp the back of the calcaneus, where the achilles tendon is. Take the calcaneus into inferior distraction to maximize space between the inferior talus and the calcaneus, then abduct it repeatedly at end-range 30 times. In performing calcaneal abduction the front of the calcaneus is moving laterally. Therefore, the posterior aspect of the calcaneues moves towards midline (back of the left heel moves toward the right, back of the right heel moves left). Magic! Retest calcaneal tilt (valgus) and it will be noticeably improved. It is very rare that I am unable to restore normal calcaneal motion. Teach the client to do same in weight-bearing, stacking internal rotation throguhout the lower extremity, and actively enhancing functional pronation. Image a line connecting the hip, the knee, the ankle. repeat the exercise going from supination into full pronation and back, repeating 30-100 times. It is easily done 100x in 2-3 minutes. Strenthening is easily achieved by adding resistance tubing, etc.
Rules for Treating Cuboid Syndrome: Hands-On Joint Mobilization
1. Realizing that the calcaneus has a profound mechanical input to the cuboid, it is necessary to treat calcaneal (subtalar) restrictions, such as lack of normative eversion/valgus.
2. The navicular is second influence on the cuboid, assure that the mid foot has normal pronation through the rotation of the navicular.
3. The talus has a small influence as well, treat it if motion restriction present in any plane.
4. Type II Cuboid Syndrome involves all of the major joints of the foot and ankjle, restore all normative passive accessory motions.
5. Treat the whole kinetic chain. The hip has a significant influence on weight bearing through the foot. stand and rotate your pelvis, it will be readily apparent.
I think that I might be one of the first to name the abduction (transverse plane rotation of the calcaneus on the talus at the subtalar joint) as a necessary motion in restoring calcaneal valgus (late 1980's) - I just stumbled on it many years ago in the clinic - but if you have a reference that says otherwise, please let me know. I will be happy to post it. I have done literature searches but have not encountered that statement. I went to do a web search to find a quotable definition of cuboid syndrome and came upon my post on the topic from 2006. Taken from Physiobase* www.physiobase.com Please see their privacy policy below, at the very bottome of this entire post. I do not believe that I am in violation by posting this. I did clean it up a little and added some.
(18/2/06 3:59 am)
Jerry's Reply
Cuboid
Good answers are the topic of cuboid syndrome. I have treated this for 2 decades, so I have some thoughts. I intended to submit a letter to the editor after the article cited earlier in JOSPT in 2005, but never did. In my opinion, there are essentially 2 basic types of cuboid syndrome. I do not believe that this has been adequately addressed in the literature. For convenience I am going to name one type a TYPE I CUBOID SYNDROME and the othera TYPE II CUBOID SYNDROME.
Type I can be symptomatic or asymptomatic. It responds beautifully to a manipulation of the cuboid, and the cuboid alone. If painful, the pain resolves very quickly and the treatment is repeated if necessary, 1 or 2 times. Client and clinician are both happy. Recovery is quick. Basically the cuboid fixation is the key lesion in the foot and ankle complex and restoring mobility directly to the cuboid makes for significant improvement. Sometimes there is a pattern that appears to involve several other structures in the foot and ankle, yet the manipulation performed only at the cuboid, is almost magical. Retesting the other motion fixations reveals that they are also remarkably improved and they do not require treatment. I affectionately and metaphoriclly refer to the cuboid as "1/2 of a keystone." It has no lateral structure to articulate with, as it is the most lateral of that row of mid foot bones. When it subluxes laterally with foot and ankle in inversion, there is much to hold it out there, the articulating lateral cunieform and the articulating calcaneus. The navicular also articulates with the cuboid, and the 4th and 5th metatarsals proably play a rather minor role. It is very helpful to have a foot and ankle model that includes the whole foot and a short portion of the distal tibia and fibula, of course talus and calcaneus included. Take apart the joint leaving the forefoot, the cuneoforms, the navicular and the cuboid as one and the talus and calcaneus are seperate (as is their attachment to the distal tibia and fibula. It is so helpful to learning, to have this semi-disarticulated model in hand. You can put the pieces together and observe how the bones interact. It should be easy to perceive how the cuboid is "out there by itself" being most lateral and it is easy to see how it could be elevated (vertical axis) and laterally rotated about an A-P axis, remaining stuck in an inversion injury.
The cuboid can be palpated and compared to the unaffected side. Typically it is more prominent on the painful side and inferior glide spring testing and "pronatory" spring testing reveal fixation (and discomfort). I do not believe that one can NOT accurately perform a superior glide spring test due to thickness of the soft tissue on the plantar surface of the foot. The typical manipulation is opposite to the way I prefer to mobilize it. The typical manipulation involves a superior thrust from the plantar surface of the foot, see details in other post, below. The typical manipulation appears to enhance the lesion - yet gap the joint and I believe that it recoils back to normal position. I prefer to mobilize it with progressive inferior glide (dorsal to plantar direction)and add medial rotation mobilization, while I attempt to "create space" and coax it back by taking the navicular and the cuboids into medial glide and medial rotation.
Now a description of what I conveniently refer to as TYPE II CUBOID SYNDROME. This can be symptomatic or asymptomatic, with all grades in between from acute to chronic. The difference is that a supinatory pattern of the foot and ankle complex has set in and efforts to mobilize only the cuboid will fail miserably, will not provide that quick fix, described earlier. Instead, you have to treat all major articulations and this is where we get into some controversy. This same pattern is commonly encountered in recurrent ankle sprains. I find restrictions (in the oppsite directions) and restore mobility in the following directions:
MAJOR MOTIONS OF THE FOOT AND ANKLE:
Sometimes just before the final mob to the calcaneus I will evaluate and treat if needed, medial glide to the talus working through the distal fibula and just below it as well. After all of the above I go into a weight-bearing context and adress those motions that I can - if I find them to be restricted in weight bearing, such as distal tibia rotation, calcaneal valgus, etc. I teach the client to internally rotate from hip down to distal tibia and gently, repeatedly self-mobilize into pronation 30-100 reps, daily for a week and then as needed.
There are other flavors in which there is enough laxity in the ligaments that the above is not effective, fortunatley these are in the minority and I am not referrring to this sub-population is this commentary. There is a great need for more research on the above topic and I think that our profession does not typically look at structures as patterns of motion dysfunction. The Cuboid Syndrome a perfect example in which only one dysfunctional structure (the cuboid) is mentioned and only mobilization to that singular structure is described. I have made a case for Type II Cuboid Syndrome being a much more complex pattern that requires a dozen or more sequential mobility screens and treatment with mobilization. Terms like hypermobility and hypomobility get tossed around in the literature without adequate clarification, without explaining in detail, the tests are used with the cuboid.
After restoring normal motion, stability, strength, blance, endurance, proprioception, etc it is very appropriate to look up the kinetic chain and find out where the body has adapted or compensated for this pattern and treat what you find. Typically I end up treating the pelvis/SI and upper cervical spine, though if the pattern is not chronic; the distal compensation may reflexively resolve with no direct effort on my part. I hope this has been additive to the body of knowledge. There are some very good articles in the recent literature to guide rehabilitation, such as in JOSPT 2007.
Jerry Hesch, MHS, PT
[email protected]
By: Dr. Jeffrey A. Oster, Medical Director Of www.Myfootshop.com Cuboid syndrome refers to the disruption of the normal function of the calcaneal-cuboid joint (CC joint). Disruption of the CC joint is often called subluxation. Cuboid syndrome can be found described in the literature as a sequella of inversion sprains of the ankle. Also, cuboid syndrome is found described in dance (ballet) literature.
Cuboid syndrome is somewhat uncommon and is poorly defined in the literature. When conditions are poorly defined in the literature, this usually means that there is a lack of agreement among doctors as to the eitiology (reason for the condition) and the treatment.
Treatment Of Cuboid Syndrome
Cuboid syndrome is treated by reducing (realigning) the subluxation of the CC joint and stabilizing the reduction. Reduction of the subluxation can be accomplished by manipulating the joint. Manipulation is performed with the patient in a prone (face down) position. The doctor cradles the foot in his/her hands and places both thumbs beneath the CC joint. The CC joint is then manipulated by a forceful movement, moving the leg at the knee and the ankle while applying pressure with the thumbs at the plantar (bottom) aspect of the CC joint.
Reduction of the subluxation can be maintained with taping, and padding. Prescription orthotics (arch supports) are helpful in preventing a recurrence of cuboid syndrome. Occasionally, cortisone injections may be helpful in reducing inflammation associated with the subluxation of the CC joint. Patients are instructed to avoid going barefoot or wearing shoes with low heels. Small (less that 1/2") heel lifts can also be helpful.
Chronic cuboid syndrome is called tarsitis (inflammation of the tarsal bones). Tarsitis results from excessive intrinsic load, often called CT band syndrome. Tarsitis is just one of many symptoms of CT band syndrome. For additional information regarding chronic cuboid syndrome (tarsitis), please read our article on CT band syndrome.
The response to treatment of cuboid syndrome depends upon the eitiology and onset of symptoms. Acute onset of cuboid syndrome, say from an ankle sprain, may respond dramatically to manipulation. If cuboid syndrome is due to chronic, excessive intrinsic load (CT band syndrome) treatment such as manipulation may be less effective and take longer to see results.
Nomenclature:
Cuboid - named after its' square shape. The cuboid has historically been used in games as a dice.
Chopart's Joint - includes the talo-navicular joint and the calcaneal-cuboid joint. Named after the French surgeon Francois Chopart (1743-1795).
CT band - 'calf to toes' band. Describes a band consisting of the calf, Achilles tendon, ankle and plantar fascia.
Extrinsic load - any load delivered to the foot that is exclusive of intrinsic load. Extrinsic load includes the duration of time on your fee, number of steps taken in a day, body weight, etc.
Intrinsic load - load that is intrinsic to the normal mechanical function of the leg and foot. Most intrinsic load is derived from the calf and delivered to the foot via the Achilles tendon. Other sources of intrinsic load include the other plantar flexor muscles and tendons of the foot such as the peroneals and posterior tibialis.
Subluxation - motion of a joint that is irregular and not in alignment with the normal range of motion of the joint.
Tarsal bone - the large bones of the rear foot including the calcaneus, talus, navicular and cuboid.
Anatomy:
The calcaneal-cuboid joint (CC joint) is located on the lateral (outside) aspect of the foot. The CC joint can be found immediately below the outside of the ankle and about two fingers distal (towards the toes). The CC joint is a broad, flat joint build to bear load. The joint has very little movement or motion. The CC joint is surrounded by a number of stout ligaments that are intended to limit motion and stabilize the joint. On the plantar aspect (bottom) of the joint are the long plantar ligament and calcaneal-cuboid ligament. The lateral side (outside) of the joint is stabilized by the dorsal calcaneal-cuboid ligament. The dorsal aspect (top) of the cuboid is stabilized by the dorsal cuneo-cuboid ligament, the tarso-metatarsal ligaments, dorsal cuboideo-navicular ligament and miscellaneous inter-tarsal ligaments.
The CC joint is also stabilized by a number of contiguous structures that pass above, below or along the cuboid. The most significant of these is the peroneus longus tendon that wraps along the lateral and plantar aspects of the cuboid. The cuboid is essentially help in a sling by the peroneus longus tendon. Other structures include the peroneus brevis tendon, dorsal and plantar musculature and retinaculum.
Biomechanics:
Cuboid syndrome occurs at the calcaneal-cuboid joint (CC joint) on the lateral or outside of the foot. The CC joint functions together with the talo-navicular joint (TN joint) and the subtalar joint (STJ) to deliver load to the forefoot. The function of these joints is to deliver load that can be converted into action; walking, running etc. For additional definitions of load in relationship to the normal function of the foot and leg, please refer to our article on CT band syndrome.
Cuboid syndrome occurs when the calcaneal-cuboid joint is unable to carry the load that is applied to it. The result is that the calcaneal-cuboid joint subluxes (moves out of its' normal position).
Symptoms:
The onset of cuboid syndrome may be due to an acute injury of the lower extremity such as an inversion sprain of the ankle. Occasionally the symptoms of cuboid syndrome occur without an obvious injury. The symptoms of cuboid syndrome are very similar to the symptoms of a sprain. Pain is significant when weight is first applied to the foot. Pain increases with the toe off phase of gait as the weight of the body and load from the calf muscle are delivered to the lateral (outside) column of the foot.
Cuboid syndrome rarely presents with bruising or swelling. The location of cuboid syndrome (at the calcaneal cuboid joint) can be pin pointed by this simple method; visualize a line extending from the outside ankle bone (fibula) to the floor. The calcaneal cuboid joint is approximately two fingers from this line distal (towards the toes).
Differential Diagnosis:
Calcaneal stress fracture
Sinus tarsi syndrome
Peroneal tendonitis
Partial peroneal tendon rupture
5th metatarsal avulsion fracture
Compression neuropathy of the sural nerve
Cuboid fracture
Os peroneum
Gout
Tarsal coalition
Tarsitis
References:
1. Stone DA, Kamenski R, Shaw J, Nachazel KMJ, Conti SF, Fu FH. Sports Injuries, Mechanics, Prevention, Treatment-Second Edition. Philadelphia, Lippincott Williams and Wilkin; 2001. pp381-397.
2. Leerar, PJ. Differential Diagnosis of Tarsal Coalition versus Cuboid Syndrome In An Adolescent Athlete. J Orthop Sports Phys Ther 2001; 31(12)
3. Marshall P, Hamilton WG. Cuboid Subluxation In Ballet Dancers. Am J Sport Med 1992; 20(2).
4. Mooney M, Maffey-Ward L. Cuboid Plantar And Dorsal Subluxations: Assesment And Treatment. J Ortho Sports Phys Ther 1994; 20(4).
About the author:
Jeffrey A. Oster, DPM, C.Ped is a board certified foot and ankle surgeon. Dr. Oster is also board certified in pedorthics. Dr. Oster is medical director of www.Myfootshop.com and is in active practice in Granville, Ohio.
*Security and Privacy
The following notice applies to all information, services, products, software, mailing lists,and other materials posted on the World Wide Web pages of Physiobase.com at www.physiobase.com
Physiobase.com maintains a strict privacy policy. Under no circumstances will any user information not intended for public display be directly given, sold or exchanged to third parties seeking such information. Physiobase and it's affiliate businesses may from time to time communicate with our members offering information about third party products and services. This however is an in-house direct communication channel and no member information has been passed on to any third party. All members have the right to be removed from our mailing service by replying to any education or promotional material using the remove or unsubscribe options attached to all correspondence.
Personal details are accessible only via the use of a valid username and password combination and can be accessed only by the member themselves or the website administrators.
Unless otherwise indicated, the copyright in all of the materials available on this web site belong to the author. All rights reserved. Except as expressly set forth below, the content of this Web site may not be republished, reproduced, transmitted, or distributed, whether mechanically, electronically, or in any other medium, without prior written approval from the author or Physiobase.com. Commercial reproduction and multiple distribution or publication, in any form or medium, is prohibited.
Individuals or educational institutions may reproduce content from this web site for non-commercial, educational or personal purposes only, in accordance with "fair use" principles under copyright law. Copies of any portion of the content of this web site must include a notice that such content is "Copyrighted by Physiobase.com."
All trademarks and service marks appearing on this web site are the property of their respective owners.
2. The navicular is second influence on the cuboid, assure that the mid foot has normal pronation through the rotation of the navicular.
3. The talus has a small influence as well, treat it if motion restriction present in any plane.
4. Type II Cuboid Syndrome involves all of the major joints of the foot and ankjle, restore all normative passive accessory motions.
5. Treat the whole kinetic chain. The hip has a significant influence on weight bearing through the foot. stand and rotate your pelvis, it will be readily apparent.
I think that I might be one of the first to name the abduction (transverse plane rotation of the calcaneus on the talus at the subtalar joint) as a necessary motion in restoring calcaneal valgus (late 1980's) - I just stumbled on it many years ago in the clinic - but if you have a reference that says otherwise, please let me know. I will be happy to post it. I have done literature searches but have not encountered that statement. I went to do a web search to find a quotable definition of cuboid syndrome and came upon my post on the topic from 2006. Taken from Physiobase* www.physiobase.com Please see their privacy policy below, at the very bottome of this entire post. I do not believe that I am in violation by posting this. I did clean it up a little and added some.
(18/2/06 3:59 am)
Jerry's Reply
Cuboid
Good answers are the topic of cuboid syndrome. I have treated this for 2 decades, so I have some thoughts. I intended to submit a letter to the editor after the article cited earlier in JOSPT in 2005, but never did. In my opinion, there are essentially 2 basic types of cuboid syndrome. I do not believe that this has been adequately addressed in the literature. For convenience I am going to name one type a TYPE I CUBOID SYNDROME and the othera TYPE II CUBOID SYNDROME.
Type I can be symptomatic or asymptomatic. It responds beautifully to a manipulation of the cuboid, and the cuboid alone. If painful, the pain resolves very quickly and the treatment is repeated if necessary, 1 or 2 times. Client and clinician are both happy. Recovery is quick. Basically the cuboid fixation is the key lesion in the foot and ankle complex and restoring mobility directly to the cuboid makes for significant improvement. Sometimes there is a pattern that appears to involve several other structures in the foot and ankle, yet the manipulation performed only at the cuboid, is almost magical. Retesting the other motion fixations reveals that they are also remarkably improved and they do not require treatment. I affectionately and metaphoriclly refer to the cuboid as "1/2 of a keystone." It has no lateral structure to articulate with, as it is the most lateral of that row of mid foot bones. When it subluxes laterally with foot and ankle in inversion, there is much to hold it out there, the articulating lateral cunieform and the articulating calcaneus. The navicular also articulates with the cuboid, and the 4th and 5th metatarsals proably play a rather minor role. It is very helpful to have a foot and ankle model that includes the whole foot and a short portion of the distal tibia and fibula, of course talus and calcaneus included. Take apart the joint leaving the forefoot, the cuneoforms, the navicular and the cuboid as one and the talus and calcaneus are seperate (as is their attachment to the distal tibia and fibula. It is so helpful to learning, to have this semi-disarticulated model in hand. You can put the pieces together and observe how the bones interact. It should be easy to perceive how the cuboid is "out there by itself" being most lateral and it is easy to see how it could be elevated (vertical axis) and laterally rotated about an A-P axis, remaining stuck in an inversion injury.
The cuboid can be palpated and compared to the unaffected side. Typically it is more prominent on the painful side and inferior glide spring testing and "pronatory" spring testing reveal fixation (and discomfort). I do not believe that one can NOT accurately perform a superior glide spring test due to thickness of the soft tissue on the plantar surface of the foot. The typical manipulation is opposite to the way I prefer to mobilize it. The typical manipulation involves a superior thrust from the plantar surface of the foot, see details in other post, below. The typical manipulation appears to enhance the lesion - yet gap the joint and I believe that it recoils back to normal position. I prefer to mobilize it with progressive inferior glide (dorsal to plantar direction)and add medial rotation mobilization, while I attempt to "create space" and coax it back by taking the navicular and the cuboids into medial glide and medial rotation.
Now a description of what I conveniently refer to as TYPE II CUBOID SYNDROME. This can be symptomatic or asymptomatic, with all grades in between from acute to chronic. The difference is that a supinatory pattern of the foot and ankle complex has set in and efforts to mobilize only the cuboid will fail miserably, will not provide that quick fix, described earlier. Instead, you have to treat all major articulations and this is where we get into some controversy. This same pattern is commonly encountered in recurrent ankle sprains. I find restrictions (in the oppsite directions) and restore mobility in the following directions:
MAJOR MOTIONS OF THE FOOT AND ANKLE:
- posterior glide of the talus - the method also mobilizes the calcaneus anteriorly at the same time
- medial rotation of the talus
- +/- internal rotation of the talus
- +/- posterior glide of distal tibia
- +/- medial rotation of distal tibia
- posterior glide of the distal malleolus (on rare occasions it is found to be stuck posteriorly thus mobilized nteriorly)
- +/- ant or post glide of fibular head
- superior glide of the fibula (not described in the bulk of the literature, but indeed a very relevant, seperate accessory motion - great research project) This does NOT self-correct as a coupled motion with mobilization/Muscle Energy in A-P, or P-A directions.
- inferior glide and medial rotation of the navicular and then incorporating the cunieoforms
- inferior glide and medial rotation/medial glide to the cuboid
- superior/inferior glide to base of 5th metatarsal
- last but not least is the calcaneus:
Sometimes just before the final mob to the calcaneus I will evaluate and treat if needed, medial glide to the talus working through the distal fibula and just below it as well. After all of the above I go into a weight-bearing context and adress those motions that I can - if I find them to be restricted in weight bearing, such as distal tibia rotation, calcaneal valgus, etc. I teach the client to internally rotate from hip down to distal tibia and gently, repeatedly self-mobilize into pronation 30-100 reps, daily for a week and then as needed.
There are other flavors in which there is enough laxity in the ligaments that the above is not effective, fortunatley these are in the minority and I am not referrring to this sub-population is this commentary. There is a great need for more research on the above topic and I think that our profession does not typically look at structures as patterns of motion dysfunction. The Cuboid Syndrome a perfect example in which only one dysfunctional structure (the cuboid) is mentioned and only mobilization to that singular structure is described. I have made a case for Type II Cuboid Syndrome being a much more complex pattern that requires a dozen or more sequential mobility screens and treatment with mobilization. Terms like hypermobility and hypomobility get tossed around in the literature without adequate clarification, without explaining in detail, the tests are used with the cuboid.
After restoring normal motion, stability, strength, blance, endurance, proprioception, etc it is very appropriate to look up the kinetic chain and find out where the body has adapted or compensated for this pattern and treat what you find. Typically I end up treating the pelvis/SI and upper cervical spine, though if the pattern is not chronic; the distal compensation may reflexively resolve with no direct effort on my part. I hope this has been additive to the body of knowledge. There are some very good articles in the recent literature to guide rehabilitation, such as in JOSPT 2007.
Jerry Hesch, MHS, PT
[email protected]
By: Dr. Jeffrey A. Oster, Medical Director Of www.Myfootshop.com Cuboid syndrome refers to the disruption of the normal function of the calcaneal-cuboid joint (CC joint). Disruption of the CC joint is often called subluxation. Cuboid syndrome can be found described in the literature as a sequella of inversion sprains of the ankle. Also, cuboid syndrome is found described in dance (ballet) literature.
Cuboid syndrome is somewhat uncommon and is poorly defined in the literature. When conditions are poorly defined in the literature, this usually means that there is a lack of agreement among doctors as to the eitiology (reason for the condition) and the treatment.
Treatment Of Cuboid Syndrome
Cuboid syndrome is treated by reducing (realigning) the subluxation of the CC joint and stabilizing the reduction. Reduction of the subluxation can be accomplished by manipulating the joint. Manipulation is performed with the patient in a prone (face down) position. The doctor cradles the foot in his/her hands and places both thumbs beneath the CC joint. The CC joint is then manipulated by a forceful movement, moving the leg at the knee and the ankle while applying pressure with the thumbs at the plantar (bottom) aspect of the CC joint.
Reduction of the subluxation can be maintained with taping, and padding. Prescription orthotics (arch supports) are helpful in preventing a recurrence of cuboid syndrome. Occasionally, cortisone injections may be helpful in reducing inflammation associated with the subluxation of the CC joint. Patients are instructed to avoid going barefoot or wearing shoes with low heels. Small (less that 1/2") heel lifts can also be helpful.
Chronic cuboid syndrome is called tarsitis (inflammation of the tarsal bones). Tarsitis results from excessive intrinsic load, often called CT band syndrome. Tarsitis is just one of many symptoms of CT band syndrome. For additional information regarding chronic cuboid syndrome (tarsitis), please read our article on CT band syndrome.
The response to treatment of cuboid syndrome depends upon the eitiology and onset of symptoms. Acute onset of cuboid syndrome, say from an ankle sprain, may respond dramatically to manipulation. If cuboid syndrome is due to chronic, excessive intrinsic load (CT band syndrome) treatment such as manipulation may be less effective and take longer to see results.
Nomenclature:
Cuboid - named after its' square shape. The cuboid has historically been used in games as a dice.
Chopart's Joint - includes the talo-navicular joint and the calcaneal-cuboid joint. Named after the French surgeon Francois Chopart (1743-1795).
CT band - 'calf to toes' band. Describes a band consisting of the calf, Achilles tendon, ankle and plantar fascia.
Extrinsic load - any load delivered to the foot that is exclusive of intrinsic load. Extrinsic load includes the duration of time on your fee, number of steps taken in a day, body weight, etc.
Intrinsic load - load that is intrinsic to the normal mechanical function of the leg and foot. Most intrinsic load is derived from the calf and delivered to the foot via the Achilles tendon. Other sources of intrinsic load include the other plantar flexor muscles and tendons of the foot such as the peroneals and posterior tibialis.
Subluxation - motion of a joint that is irregular and not in alignment with the normal range of motion of the joint.
Tarsal bone - the large bones of the rear foot including the calcaneus, talus, navicular and cuboid.
Anatomy:
The calcaneal-cuboid joint (CC joint) is located on the lateral (outside) aspect of the foot. The CC joint can be found immediately below the outside of the ankle and about two fingers distal (towards the toes). The CC joint is a broad, flat joint build to bear load. The joint has very little movement or motion. The CC joint is surrounded by a number of stout ligaments that are intended to limit motion and stabilize the joint. On the plantar aspect (bottom) of the joint are the long plantar ligament and calcaneal-cuboid ligament. The lateral side (outside) of the joint is stabilized by the dorsal calcaneal-cuboid ligament. The dorsal aspect (top) of the cuboid is stabilized by the dorsal cuneo-cuboid ligament, the tarso-metatarsal ligaments, dorsal cuboideo-navicular ligament and miscellaneous inter-tarsal ligaments.
The CC joint is also stabilized by a number of contiguous structures that pass above, below or along the cuboid. The most significant of these is the peroneus longus tendon that wraps along the lateral and plantar aspects of the cuboid. The cuboid is essentially help in a sling by the peroneus longus tendon. Other structures include the peroneus brevis tendon, dorsal and plantar musculature and retinaculum.
Biomechanics:
Cuboid syndrome occurs at the calcaneal-cuboid joint (CC joint) on the lateral or outside of the foot. The CC joint functions together with the talo-navicular joint (TN joint) and the subtalar joint (STJ) to deliver load to the forefoot. The function of these joints is to deliver load that can be converted into action; walking, running etc. For additional definitions of load in relationship to the normal function of the foot and leg, please refer to our article on CT band syndrome.
Cuboid syndrome occurs when the calcaneal-cuboid joint is unable to carry the load that is applied to it. The result is that the calcaneal-cuboid joint subluxes (moves out of its' normal position).
Symptoms:
The onset of cuboid syndrome may be due to an acute injury of the lower extremity such as an inversion sprain of the ankle. Occasionally the symptoms of cuboid syndrome occur without an obvious injury. The symptoms of cuboid syndrome are very similar to the symptoms of a sprain. Pain is significant when weight is first applied to the foot. Pain increases with the toe off phase of gait as the weight of the body and load from the calf muscle are delivered to the lateral (outside) column of the foot.
Cuboid syndrome rarely presents with bruising or swelling. The location of cuboid syndrome (at the calcaneal cuboid joint) can be pin pointed by this simple method; visualize a line extending from the outside ankle bone (fibula) to the floor. The calcaneal cuboid joint is approximately two fingers from this line distal (towards the toes).
Differential Diagnosis:
Calcaneal stress fracture
Sinus tarsi syndrome
Peroneal tendonitis
Partial peroneal tendon rupture
5th metatarsal avulsion fracture
Compression neuropathy of the sural nerve
Cuboid fracture
Os peroneum
Gout
Tarsal coalition
Tarsitis
References:
1. Stone DA, Kamenski R, Shaw J, Nachazel KMJ, Conti SF, Fu FH. Sports Injuries, Mechanics, Prevention, Treatment-Second Edition. Philadelphia, Lippincott Williams and Wilkin; 2001. pp381-397.
2. Leerar, PJ. Differential Diagnosis of Tarsal Coalition versus Cuboid Syndrome In An Adolescent Athlete. J Orthop Sports Phys Ther 2001; 31(12)
3. Marshall P, Hamilton WG. Cuboid Subluxation In Ballet Dancers. Am J Sport Med 1992; 20(2).
4. Mooney M, Maffey-Ward L. Cuboid Plantar And Dorsal Subluxations: Assesment And Treatment. J Ortho Sports Phys Ther 1994; 20(4).
About the author:
Jeffrey A. Oster, DPM, C.Ped is a board certified foot and ankle surgeon. Dr. Oster is also board certified in pedorthics. Dr. Oster is medical director of www.Myfootshop.com and is in active practice in Granville, Ohio.
*Security and Privacy
The following notice applies to all information, services, products, software, mailing lists,and other materials posted on the World Wide Web pages of Physiobase.com at www.physiobase.com
Physiobase.com maintains a strict privacy policy. Under no circumstances will any user information not intended for public display be directly given, sold or exchanged to third parties seeking such information. Physiobase and it's affiliate businesses may from time to time communicate with our members offering information about third party products and services. This however is an in-house direct communication channel and no member information has been passed on to any third party. All members have the right to be removed from our mailing service by replying to any education or promotional material using the remove or unsubscribe options attached to all correspondence.
Personal details are accessible only via the use of a valid username and password combination and can be accessed only by the member themselves or the website administrators.
Unless otherwise indicated, the copyright in all of the materials available on this web site belong to the author. All rights reserved. Except as expressly set forth below, the content of this Web site may not be republished, reproduced, transmitted, or distributed, whether mechanically, electronically, or in any other medium, without prior written approval from the author or Physiobase.com. Commercial reproduction and multiple distribution or publication, in any form or medium, is prohibited.
Individuals or educational institutions may reproduce content from this web site for non-commercial, educational or personal purposes only, in accordance with "fair use" principles under copyright law. Copies of any portion of the content of this web site must include a notice that such content is "Copyrighted by Physiobase.com."
All trademarks and service marks appearing on this web site are the property of their respective owners.