Low Back Pain Case Study Letters to the Editor – Jerry Hesch, MHS, PT
March 10, 2010 Jerry's letter to the editor in response to an online post. His letter is first, the case study follows. march 26, 2010, the author's reply and Jerry's 2nd letter is below:
http://www.spineuniverse.com/professional/case-studies/dionne/back-pain-adult-cerebral-palsy?utm_source=eNewsletter&utm_medium=email&utm_campaign=SpineMonitor-03-10-2010
Hi,
Thank Carol and Don, you for the sucessful and interesting case study. The success speaks well of the chosen intervention. However, my curiosity begs a little more info and I have a a few additional thoughts. I am disinclined to ascribe the pain districution as an L4 dermatome, (though overlap is not too uncommon), I am more inclined to think of it in terms of primarily a L3 dermatome. Injuries to the L3 disc are quite rare, and I can't help but wonder if some other explanation might be worthy of consideration. Could she have had some iliopsoas spasm, which could compress the lateral femoral cutaneous nerve, or even femoral portion of genitofemoral? This would not be symptomatic with a hip scour test. What was her hip extension prior to treatment? I can see how the treatment could enhance hip extension and lengthen a tight iliopsoas complex. I also think that a facet syndrome could refer similarly, and the mechanical treatement be very effective in mobilizing a facet, strained in flexion, rotation and side bending. That one can have a generator of pain refer pain elsewhere, with the referred pain being greater than the proximal, or even overshadowing the proximal, is not too uncommon. The treatment was appropriate and the results stand alone. Nonetheless, I wonder if perhaps there are alternate considerations.
Thank you for allowing me to pose these questions.
Sincerely,
Jerry Hesch, MHS, PT
The Hesch Method, Hesch Manual Therapy
Back Pain in an Adult with Cerebral Palsy Carol P. Dionne, PT, DPT, PhD, OCS, Cert MDT Assistant Professor, Dept. Rehabilitative Sciences University of Oklahoma Health Sciences Center Oklahoma City, OK Don Stover, PT, OCS, Cert MDT Physical Therapist Stover Physical Therapy Oklahoma CIty, OK
Patient History & Diagnosis
Suggested Treatment
Patient Outcome
Community Case Discussion (1 comment)
Forward this Case to a Colleague
History A 50 year-old female full-time student was referred to Physical Therapy by a family practice physician who diagnosed the patient with "back and hip pain." This is her first episode of back pain. The condition commenced due to lifting a heavy object and has been worsening in intensity and frequency overall. Initially, she reports the pain in the back and then her thigh.
Past Medical History: She has congenital spastic diplegia, with movement impairment that affects her lower extremities more than her upper extremities. The patient reports her symptoms are not affected by coughing and sneezing. Bladder function is normal. She states that her gait is "stiffer and slower" because of the back pain. Currently, she is not taking any medication.
It should also be noted that the patient communicates with total communication (sign and speech) due to congenital sensorineural hearing loss and chooses to not use hearing aids. (Note: The clinician is functionally conversant in this mode of communication.)
Examination Observation: The patient presents with poor sitting posture. Posture correction lessened her thigh symptoms. In standing, lumbar lordosis appeared exaggerated. No lateral shift was noted.
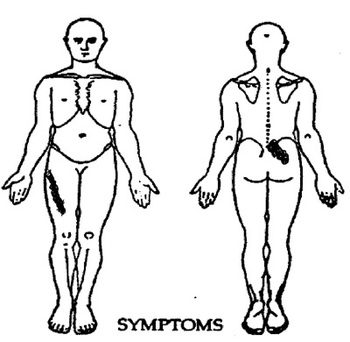
Pain: The patient reports intermittent right anterior thigh pain to mid-thigh, and constant back pain. All symptoms have been present for 4 weeks. (Fig. 1)
Figure 1. Symptoms diagram
Low Back Pain Test
March 10, 2010 Jerry's letter to the editor in response to an online post. His letter is first, the case study follows. march 26, 2010, the author's reply and Jerry's 2nd letter is below:
http://www.spineuniverse.com/professional/case-studies/dionne/back-pain-adult-cerebral-palsy?utm_source=eNewsletter&utm_medium=email&utm_campaign=SpineMonitor-03-10-2010
Hi,
Thank Carol and Don, you for the sucessful and interesting case study. The success speaks well of the chosen intervention. However, my curiosity begs a little more info and I have a a few additional thoughts. I am disinclined to ascribe the pain districution as an L4 dermatome, (though overlap is not too uncommon), I am more inclined to think of it in terms of primarily a L3 dermatome. Injuries to the L3 disc are quite rare, and I can't help but wonder if some other explanation might be worthy of consideration. Could she have had some iliopsoas spasm, which could compress the lateral femoral cutaneous nerve, or even femoral portion of genitofemoral? This would not be symptomatic with a hip scour test. What was her hip extension prior to treatment? I can see how the treatment could enhance hip extension and lengthen a tight iliopsoas complex. I also think that a facet syndrome could refer similarly, and the mechanical treatement be very effective in mobilizing a facet, strained in flexion, rotation and side bending. That one can have a generator of pain refer pain elsewhere, with the referred pain being greater than the proximal, or even overshadowing the proximal, is not too uncommon. The treatment was appropriate and the results stand alone. Nonetheless, I wonder if perhaps there are alternate considerations.
Thank you for allowing me to pose these questions.
Sincerely,
Jerry Hesch, MHS, PT
The Hesch Method, Hesch Manual Therapy
Back Pain in an Adult with Cerebral Palsy Carol P. Dionne, PT, DPT, PhD, OCS, Cert MDT Assistant Professor, Dept. Rehabilitative Sciences University of Oklahoma Health Sciences Center Oklahoma City, OK Don Stover, PT, OCS, Cert MDT Physical Therapist Stover Physical Therapy Oklahoma CIty, OK
Past Medical History: She has congenital spastic diplegia, with movement impairment that affects her lower extremities more than her upper extremities. The patient reports her symptoms are not affected by coughing and sneezing. Bladder function is normal. She states that her gait is "stiffer and slower" because of the back pain. Currently, she is not taking any medication.
It should also be noted that the patient communicates with total communication (sign and speech) due to congenital sensorineural hearing loss and chooses to not use hearing aids. (Note: The clinician is functionally conversant in this mode of communication.)
Examination Observation: The patient presents with poor sitting posture. Posture correction lessened her thigh symptoms. In standing, lumbar lordosis appeared exaggerated. No lateral shift was noted.
Pain: The patient reports intermittent right anterior thigh pain to mid-thigh, and constant back pain. All symptoms have been present for 4 weeks. (Fig. 1)
Figure 1. Symptoms diagram
http://www.spineuniverse.com/professional/case-studies/dionne/back-pain-adult-cerebral-palsy?utm_source=eNewsletter&utm_medium=email&utm_campaign=SpineMonitor-03-10-2010
Hi,
Thank Carol and Don, you for the sucessful and interesting case study. The success speaks well of the chosen intervention. However, my curiosity begs a little more info and I have a a few additional thoughts. I am disinclined to ascribe the pain districution as an L4 dermatome, (though overlap is not too uncommon), I am more inclined to think of it in terms of primarily a L3 dermatome. Injuries to the L3 disc are quite rare, and I can't help but wonder if some other explanation might be worthy of consideration. Could she have had some iliopsoas spasm, which could compress the lateral femoral cutaneous nerve, or even femoral portion of genitofemoral? This would not be symptomatic with a hip scour test. What was her hip extension prior to treatment? I can see how the treatment could enhance hip extension and lengthen a tight iliopsoas complex. I also think that a facet syndrome could refer similarly, and the mechanical treatement be very effective in mobilizing a facet, strained in flexion, rotation and side bending. That one can have a generator of pain refer pain elsewhere, with the referred pain being greater than the proximal, or even overshadowing the proximal, is not too uncommon. The treatment was appropriate and the results stand alone. Nonetheless, I wonder if perhaps there are alternate considerations.
Thank you for allowing me to pose these questions.
Sincerely,
Jerry Hesch, MHS, PT
The Hesch Method, Hesch Manual Therapy
Back Pain in an Adult with Cerebral Palsy Carol P. Dionne, PT, DPT, PhD, OCS, Cert MDT Assistant Professor, Dept. Rehabilitative Sciences University of Oklahoma Health Sciences Center Oklahoma City, OK Don Stover, PT, OCS, Cert MDT Physical Therapist Stover Physical Therapy Oklahoma CIty, OK
- Patient History & Diagnosis
- Suggested Treatment
- Patient Outcome
- Community Case Discussion (1 comment)
- Forward this Case to a Colleague
Past Medical History: She has congenital spastic diplegia, with movement impairment that affects her lower extremities more than her upper extremities. The patient reports her symptoms are not affected by coughing and sneezing. Bladder function is normal. She states that her gait is "stiffer and slower" because of the back pain. Currently, she is not taking any medication.
It should also be noted that the patient communicates with total communication (sign and speech) due to congenital sensorineural hearing loss and chooses to not use hearing aids. (Note: The clinician is functionally conversant in this mode of communication.)
Examination Observation: The patient presents with poor sitting posture. Posture correction lessened her thigh symptoms. In standing, lumbar lordosis appeared exaggerated. No lateral shift was noted.
Pain: The patient reports intermittent right anterior thigh pain to mid-thigh, and constant back pain. All symptoms have been present for 4 weeks. (Fig. 1)
Figure 1. Symptoms diagram
Function: The patient reports that the pain interferes with long-term sitting while in class, driving, donning her slacks and footwear, and turning in bed. Initial self-rating on the Oswestry Low Back Disability Index is at 34% (Moderate Disability).
Pain Behavior: Her symptoms are aggravated with sitting for prolonged time periods and rising from sitting. Walking for short periods and lying supine alleviates symptoms.
Neurological Testing: There was bilaterally generalized weakness in the hip extensors, knee extensors, and dorsiflexors. Reflex testing results showed hyper-reflexia of all knee and ankle reflexes and negative straight leg rise testing. The patient reported no changes in sensation in the lower extremities since the onset of the back pain episode.
Lumbar Movement Loss: There was minimal loss of lumbar flexion in standing with report of sharp, increased back and thigh pain. There was moderate loss of extension in standing with no effect on her symptoms. No loss in side-gliding to the right or left was noted.
Repeated Movement Testing of Lumbar Spine
In standing: Baseline symptoms: back pain, right anterolateral hip pain to mid-thigh.
Lumbar flexion in standing: increased back and right anterior thigh pain, increased with repetition, and remained worse.
Lumbar extension in standing: decreased right thigh pain with repetition, but did not remain better.
In recumbent
Baseline symptoms: back pain, right anterolateral hip pain to mid-thigh.
Lumbar flexion in supine (knees-to-chest): no effect on symptoms.
Lumbar extension in lying (press-up): decreased back or thigh pain, production of upper extremity fatigue, and no better as a result.
Hip provocative testing (e.g. hip scour test): negative
Pretreatment Images She has undergone diagnostic radiography that was reportedly "negative in results."
Back to top Suggest TreatmentIndicate how you would treat this patient by completing the following brief survey. Your response will be added to our survey results below. Back to top Diagnosis Reversible lumbar disc pathology
Selected Treatment Initial Treatment: Postural correction, avoidance of flexion and lifting, and to perform repeated lumbar extension in lying because repeated passive extension reduced and abolished the patient's symptoms.
Pain Behavior: Her symptoms are aggravated with sitting for prolonged time periods and rising from sitting. Walking for short periods and lying supine alleviates symptoms.
Neurological Testing: There was bilaterally generalized weakness in the hip extensors, knee extensors, and dorsiflexors. Reflex testing results showed hyper-reflexia of all knee and ankle reflexes and negative straight leg rise testing. The patient reported no changes in sensation in the lower extremities since the onset of the back pain episode.
Lumbar Movement Loss: There was minimal loss of lumbar flexion in standing with report of sharp, increased back and thigh pain. There was moderate loss of extension in standing with no effect on her symptoms. No loss in side-gliding to the right or left was noted.
Repeated Movement Testing of Lumbar Spine
In standing: Baseline symptoms: back pain, right anterolateral hip pain to mid-thigh.
Lumbar flexion in standing: increased back and right anterior thigh pain, increased with repetition, and remained worse.
Lumbar extension in standing: decreased right thigh pain with repetition, but did not remain better.
In recumbent
Baseline symptoms: back pain, right anterolateral hip pain to mid-thigh.
Lumbar flexion in supine (knees-to-chest): no effect on symptoms.
Lumbar extension in lying (press-up): decreased back or thigh pain, production of upper extremity fatigue, and no better as a result.
Hip provocative testing (e.g. hip scour test): negative
Pretreatment Images She has undergone diagnostic radiography that was reportedly "negative in results."
Back to top Suggest TreatmentIndicate how you would treat this patient by completing the following brief survey. Your response will be added to our survey results below. Back to top Diagnosis Reversible lumbar disc pathology
Selected Treatment Initial Treatment: Postural correction, avoidance of flexion and lifting, and to perform repeated lumbar extension in lying because repeated passive extension reduced and abolished the patient's symptoms.
Repeated end-range extension (Figure 2A, 2B): 50 repetitions of repeated passive trunk extension decreased, abolished back and thigh pain, better as a result symptomatically and functionally.
The patient was instructed to (1) perform repeated lumbar extension (10 repetitions) in lying 4 to 6 times per day, (2) avoid flexion-biased activity (e.g., sitting, bending), (3) maintain proper posture (with maintenance of lumbar lordosis), and (4) return 2 days later for reassessment.
During the second session, her thigh symptoms ended and back symptoms were occasional. The patient required further instruction on proper performance of repeated extension in prone.
Reassessment of her symptomatic and mechanical responses to movement testing was reassessed over that visit, the third session, and 2 days later.
The patient was instructed to (1) perform repeated lumbar extension (10 repetitions) in lying 4 to 6 times per day, (2) avoid flexion-biased activity (e.g., sitting, bending), (3) maintain proper posture (with maintenance of lumbar lordosis), and (4) return 2 days later for reassessment.
During the second session, her thigh symptoms ended and back symptoms were occasional. The patient required further instruction on proper performance of repeated extension in prone.
Reassessment of her symptomatic and mechanical responses to movement testing was reassessed over that visit, the third session, and 2 days later.
Low Back Pain Test Results
(1) Lumbar extension in standing was full and painless.
(2) Lumbar flexion in standing was full but slowly performed.
At the conclusion of the third session, the patient claimed she was more aware of assumption of proper posture and able to sit in school without pain. She could roll over in bed with "a little soreness" but, all symptoms ended with regular extension exercises, which she would periodically perform throughout the day. Gait had improved in quality and cadence.
Outcome The patient accomplished treatment goals after 3 visits over a period of 5 days. She was discharged from physical therapy.
Author's Discussion This patient's symptoms centralized and ended with repeated movement testing in extension. She was classified as a rapid responder, likely due to reversible disc pathology (reducible derangement). This method of examination, Mechanical Diagnosis and Therapy (MDT), has been shown to reliably and quickly identify patients whose back and/or leg pain emanates from the spine and who are capable of responding to conservative care. Also, this case shows that those with upper extremity weakness need repeated extension in lying (via REPEX) to effectively reduce mechanical back pain may benefit from repeated end-range extension. This case presents good evidence of the ability for specially-trained physical therapists to manage most activity-related spine disorders, including those with unrelated congenital movement impairment, such as cerebral palsy. Like the vast majority of people who experience mechanical back pain, this patient responded rapidly to appropriate mechanical therapy and required no further intervention. References
1. Aina A, May S, Clare H. The centralization phenomenon of spinal symptoms - a systematic review. Man Ther; Aug;9(3):134-143, 2004.
2. Alexander LA, Hancock E, Agouris I, Smith FW, MacSween A. The response of the nucleus pulposus of the lumbar intervertebral discs to functionally loaded positions. Spine; 32:1508-1512, 2007.
3. Dionne CP, Herbowy S, Miller M, Smith S, Donelson R. Effect of REPEX in patients with low back pain. Manuelle Therapie, 8 3-9. (2004, German). Reprint. International Journal of Mechanical Diagnosis and Therapy, 2, pp.14-21.(March 2007, English).
4. Donelson R, Aprill C, Medcalf R, Grant W. A prospective study of centralization of lumbar and referred pain. A predictor of symptomatic discs and annular competence. Spine; May 15;22(10):1115-22, 1997.
5. Gonzalez M, Fernandez S, Dionne, CP. Comparison of REPEX and repeated prone trunk extension by healthy subjects. Manuelle Therapie, 8, 207-212 (2004, German). Reprint. International Journal of Mechanical Diagnosis and Therapy, 2, pp.7- 12 (March 2007, English).
6. Long A. The centralization phenomenon: its usefulness as a predictor of outcome in conservative treatment of chronic low back pain a pilot study. Spine; 20(23):2513-2521, 1995.
7. McKenzie RA, May S. The Lumbar Spine. Mechanical Diagnosis and Therapy. (Vol. 1 and 2) Spinal Publications, Waikanae, New Zealand; 2nd Edition, 2003.
8. Razmjou H, Kramer JF, Yamada R; Intertester reliability of the McKenzie evaluation in assessing patients with mechanical low-back pain. J Orthop Sports Phys Ther;Jul;30(7):368-383, 2000.
9. Skytte L, May S, Petersen P; Centralization: Its prognostic value in patients with referred symptoms and sciatica. Spine; 30:E293-E299, 2005.
10. Wetzel FT, Donelson R; The role of repeated end-range / pain response assessment in the management of symptomatic lumbar discs. Spine J; 3:146-154, 2003.
March 26, 2010
From the authors Dionne and Stover:
We thank Mr. Hersh for his comments. In this case report, an evidence-based classification system was employed to determine symptom response to a systematic examination process. This process was employed by a trained clinician who determined that the patient’s symptoms centralized and abolished. Centralization is key in predicting success with intervention that was matched to this patient’s presentation of mechanical response to application of specific forces. This patient presented with mechanical symptoms that were successfully ameliorated by mechanical means regardless of anatomic origin.
The mechanical diagnosis given to this patient represents the derangement syndrome, which was our classification in this case, is not necessarily a tissue-specific diagnosis. The McKenzie Institute defines derangement as: “ a disturbance of the normal resting position of the affected joint surfaces. Internal displacement of articular tissue of whatever origin will cause pain to remain constant until such time as the displacement is reduced, as evidenced by centralization of the symptoms associated with the distorted joint surfaces”. The disc has been used as a theoretical model to explain the cause of the clinical presentation and response to treatment, but in reality our ability to determine the exact tissue causing the pain is limited, although evidence is emerging. We respectfully question if Mr. Hersh's theory of iliopsoas spasm and compression of the lateral femoral cutaneous or genito femoral cutaneous nerve has similar support in research.
More importantly, from the patients’ perspective, is it does not matter what anatomic structure generates the symptoms. They just want to know how to make the problem go away and not come back. That is exactly what we should be focusing on delivering as well.
Carol P. Dionne, PT, DPT, PhD, OCS, Cert MDT
Don A. Stover PT, OCS, Cert. MDT
References:
(1) Fersum KV, Dankaets W, O’Sullivan PB.; Integration of sub-classification strategies in RCTs evaluating manual therapy treatment and exercise therapy for non-specific chronic low back pain: a systematic review. Br J Sports Med; doi:10.1136/bjsm.2009.063289, 2009.
(2) Fritz JM, Delitto A, Erhard RE; Comparison of classification-based physical therapy with therapy based on clinical practice guidelines for patients with acute low back pain. A RCT. Spine; 28:1363-1372, 2003.
(3) Fritz JM, Delitto A, Vignovic M, Busse RG; Interrater reliability of judgments of the centralization phenomenon and status change during movement testing in patients with low back pain. Arch Phys Med Rehabil; Jan;81(1):57-61, 2000.
(4) Hancock MJ, Maher CG, Latimer J, Spindler MF, McAuley JH, Laslett M, Bogduk N ; Systematic review of tests to identify the disc, SIJ or facet joint as the source of low back pain Eur Spine J; 16:1539-1550, 2007.
(5) Kilpikoski S, Alen M, Paatelma M, Simonen R, Heinonen A, Videman T ; Outcome comparison among working adults with centralizing low back pain: secondary analysis of a randomized controlled trial with 1-year follow-up. Advances in Physio; DOI: 10.1080/14038190902963087, 2009.
(6) Long A, Donelson R, Fung T; Does it matter which exercise? A randomized control trial of exercises for low back pain. Spine; Dec 1;29(23):2593-2602, 2004.
(7) Skytte L, May S, Petersen P; Centralization: Its prognostic value in patients with referred symptoms and sciatica Spine; 30:E293-E299, 2005.
(8) Werneke M, Hart DL:; Discriminant validity and relative precision for classifying patients with non-specific neck and back pain by anatomical pain patterns Spine; 28(2), 161-166, 2003.
(9) Werneke M, Hart DL, Resnik L, Stratford PW, Reyes A; Centralization: prevalence and effect on treatment outcomes using a standardized operational definition and measurement method. J Orthop Sports Phys Ther; 38:116-125, 2008.
(10) Young S, Aprill C, Laslett M; Correlation of clinical examination characteristics with three sources of chronic low back pain Spine; 3.460-465, 2003.
Jerry Hesch’s Reply March 26, 2010
In response to the reply from: Carol P. Dionne, PT, DPT, PhD, OCS, Cert MDT
I am in agreement with Dr Dionne’s her reply, and will elaborate in perhaps making a case for additional possibilities. Again, the outcome of the case study was very successful.
"We respectfully question if Mr. Hersh's (Hesch’s) theory of iliopsoas spasm and compression of the lateral femoral cutaneous or genito femoral cutaneous nerve has similar support in research."
The basic anatomy supports the possibility that the aforementioned nerves, which are formed within the psoas complex, can respond adversely to mechanical forces. Below are a few references on topic, though I am unaware of specific research, and have a difficult time imaging how specific research would be conducted on a live subject. However, I have a depth of empiricism. In 32 years of experiencing severe pain, I never had a single health care practitioner perform a competent evaluation of the 3 para-inguinal nerves, the ilioinguinal, iliohypogastric, and genital and femoral portions of the genitofemoral and lateral femoral cutaneous nerves. This occurred in spite of consistent subjective complaints and the use of a pain drawing, over a 32 year period. There exists a significant knowledge gap regarding peripheral neuropathies involving these nerves. Three decades post injury, when a family physician offered to perform a hernia screen, with skepticism, I obliged. This was the first time it had been offered. In my own ignorance, based on my experience of pain, I erroneously imaged a plexopathy that was non-treatable. This can be seen in Grant's Atlas of Anatomy 7th edition, fig 3-76. The hernia screen was exquisitely painful and the light bulb in my brain set off with the understanding that this was a peripheral neuropathy, hence perhaps treatable.
I developed a rudimentary 3-D pain drawing that might be helpful in diagnosing similar presentation, outlining the deep pain that cannot be visualized in traditional pain drawings. I described the internal screen, scouring the canal and spermatic cord and genital portion of genitofemoral which is proximal to the inguinal opening, as a diagnostic test, which apparently is not utilized by the medical profession. A letter from a renowned surgeon affirms the novelty of the test and is described in www.heschmanmualtherapy.com. Failing conservative care, traditional PT and Pain Management, I had a very successful triple neurectomy, though the proximal pain (within psoas to external inguinal ring) remains, albeit much less than the severe distal pain. The mechanism of injury is consistent with a stretch and compression multiple neuropathy, within the psoas and peripherally. Research is needed. In the clinical present, it is worthwhile to question presentations and look beyond a single paradigm. The results are valid in the case presentation, the theoretical construct that undergirds it can be expanded. While this case study is a successful intervention, there are others, myself included who may not be as successful, and other paradigms need to be brought to light, and researched. I welcome the opportunity to participate in research and believe it to be best accomplished with a team approach with knowledgeable educators and clinicians such as the authors of the case study. Their resources greatly exceed my own, and the need is great.
Again I submit the following: What was her hip extension prior to treatment? I can see how the treatment could enhance hip extension and lengthen a tight iliopsoas complex. The treatment was appropriate and the results stand alone. Nonetheless, I wonder if perhaps there are alternate considerations.
While I cannot specifically correlate my case with the case study, there are some overlapping consistencies that seem worthy of mention, worthy of consideration when similar presentations do not respond with traditional approaches. I believe that screening hip extension is relevant in all who present similarly.
Thank you for allowing me to pose these comments.
Sincerely,
Jerry Hesch, MHS, PT
the Hesch Method, Hesch Manual Therapy
Nerve Entrapment Syndromes of the Lower Extremity
Author: Minoo Hadjari Hollis, MD, Orthopedic Surgeon, Sound Orthopedics and Foot and Ankle Center
Coauthor(s): David E Lemay, MD, Consulting Staff, Pensacola PM&R Group, PA and Gulf Coast Orthopaedic Specialists, PA
http://emedicine.medscape.com/article/1234809-overview
Entrapment, Lateral Femoral cutaneous nerve
http://wiki.cns.org/wiki/index.php/Entrapment%2C_Lateral_Femoral_Cutaneous_Neuropathy
Handbook Of Peripheral Nerve Entrapmentsby Oscar A. Turner, Norman Taslitz (Editor), Steven Ward (Editor)Pub. Date: February 2010
http://search.barnesandnoble.com/Handbook-of-Peripheral-Nerve-Entrapments/Oscar-A-Turner/e/9780896031463
Dawson DM, Hallett M, Wilbourn AJ: “Miscellaneous uncommon syndromes of the lower extremity” 369-379 in Entrapment Neuropathies Third Edition Lippincott-Raven, Philadelphia, 1998.
(2) Lumbar flexion in standing was full but slowly performed.
At the conclusion of the third session, the patient claimed she was more aware of assumption of proper posture and able to sit in school without pain. She could roll over in bed with "a little soreness" but, all symptoms ended with regular extension exercises, which she would periodically perform throughout the day. Gait had improved in quality and cadence.
Outcome The patient accomplished treatment goals after 3 visits over a period of 5 days. She was discharged from physical therapy.
Author's Discussion This patient's symptoms centralized and ended with repeated movement testing in extension. She was classified as a rapid responder, likely due to reversible disc pathology (reducible derangement). This method of examination, Mechanical Diagnosis and Therapy (MDT), has been shown to reliably and quickly identify patients whose back and/or leg pain emanates from the spine and who are capable of responding to conservative care. Also, this case shows that those with upper extremity weakness need repeated extension in lying (via REPEX) to effectively reduce mechanical back pain may benefit from repeated end-range extension. This case presents good evidence of the ability for specially-trained physical therapists to manage most activity-related spine disorders, including those with unrelated congenital movement impairment, such as cerebral palsy. Like the vast majority of people who experience mechanical back pain, this patient responded rapidly to appropriate mechanical therapy and required no further intervention. References
1. Aina A, May S, Clare H. The centralization phenomenon of spinal symptoms - a systematic review. Man Ther; Aug;9(3):134-143, 2004.
2. Alexander LA, Hancock E, Agouris I, Smith FW, MacSween A. The response of the nucleus pulposus of the lumbar intervertebral discs to functionally loaded positions. Spine; 32:1508-1512, 2007.
3. Dionne CP, Herbowy S, Miller M, Smith S, Donelson R. Effect of REPEX in patients with low back pain. Manuelle Therapie, 8 3-9. (2004, German). Reprint. International Journal of Mechanical Diagnosis and Therapy, 2, pp.14-21.(March 2007, English).
4. Donelson R, Aprill C, Medcalf R, Grant W. A prospective study of centralization of lumbar and referred pain. A predictor of symptomatic discs and annular competence. Spine; May 15;22(10):1115-22, 1997.
5. Gonzalez M, Fernandez S, Dionne, CP. Comparison of REPEX and repeated prone trunk extension by healthy subjects. Manuelle Therapie, 8, 207-212 (2004, German). Reprint. International Journal of Mechanical Diagnosis and Therapy, 2, pp.7- 12 (March 2007, English).
6. Long A. The centralization phenomenon: its usefulness as a predictor of outcome in conservative treatment of chronic low back pain a pilot study. Spine; 20(23):2513-2521, 1995.
7. McKenzie RA, May S. The Lumbar Spine. Mechanical Diagnosis and Therapy. (Vol. 1 and 2) Spinal Publications, Waikanae, New Zealand; 2nd Edition, 2003.
8. Razmjou H, Kramer JF, Yamada R; Intertester reliability of the McKenzie evaluation in assessing patients with mechanical low-back pain. J Orthop Sports Phys Ther;Jul;30(7):368-383, 2000.
9. Skytte L, May S, Petersen P; Centralization: Its prognostic value in patients with referred symptoms and sciatica. Spine; 30:E293-E299, 2005.
10. Wetzel FT, Donelson R; The role of repeated end-range / pain response assessment in the management of symptomatic lumbar discs. Spine J; 3:146-154, 2003.
March 26, 2010
From the authors Dionne and Stover:
We thank Mr. Hersh for his comments. In this case report, an evidence-based classification system was employed to determine symptom response to a systematic examination process. This process was employed by a trained clinician who determined that the patient’s symptoms centralized and abolished. Centralization is key in predicting success with intervention that was matched to this patient’s presentation of mechanical response to application of specific forces. This patient presented with mechanical symptoms that were successfully ameliorated by mechanical means regardless of anatomic origin.
The mechanical diagnosis given to this patient represents the derangement syndrome, which was our classification in this case, is not necessarily a tissue-specific diagnosis. The McKenzie Institute defines derangement as: “ a disturbance of the normal resting position of the affected joint surfaces. Internal displacement of articular tissue of whatever origin will cause pain to remain constant until such time as the displacement is reduced, as evidenced by centralization of the symptoms associated with the distorted joint surfaces”. The disc has been used as a theoretical model to explain the cause of the clinical presentation and response to treatment, but in reality our ability to determine the exact tissue causing the pain is limited, although evidence is emerging. We respectfully question if Mr. Hersh's theory of iliopsoas spasm and compression of the lateral femoral cutaneous or genito femoral cutaneous nerve has similar support in research.
More importantly, from the patients’ perspective, is it does not matter what anatomic structure generates the symptoms. They just want to know how to make the problem go away and not come back. That is exactly what we should be focusing on delivering as well.
Carol P. Dionne, PT, DPT, PhD, OCS, Cert MDT
Don A. Stover PT, OCS, Cert. MDT
References:
(1) Fersum KV, Dankaets W, O’Sullivan PB.; Integration of sub-classification strategies in RCTs evaluating manual therapy treatment and exercise therapy for non-specific chronic low back pain: a systematic review. Br J Sports Med; doi:10.1136/bjsm.2009.063289, 2009.
(2) Fritz JM, Delitto A, Erhard RE; Comparison of classification-based physical therapy with therapy based on clinical practice guidelines for patients with acute low back pain. A RCT. Spine; 28:1363-1372, 2003.
(3) Fritz JM, Delitto A, Vignovic M, Busse RG; Interrater reliability of judgments of the centralization phenomenon and status change during movement testing in patients with low back pain. Arch Phys Med Rehabil; Jan;81(1):57-61, 2000.
(4) Hancock MJ, Maher CG, Latimer J, Spindler MF, McAuley JH, Laslett M, Bogduk N ; Systematic review of tests to identify the disc, SIJ or facet joint as the source of low back pain Eur Spine J; 16:1539-1550, 2007.
(5) Kilpikoski S, Alen M, Paatelma M, Simonen R, Heinonen A, Videman T ; Outcome comparison among working adults with centralizing low back pain: secondary analysis of a randomized controlled trial with 1-year follow-up. Advances in Physio; DOI: 10.1080/14038190902963087, 2009.
(6) Long A, Donelson R, Fung T; Does it matter which exercise? A randomized control trial of exercises for low back pain. Spine; Dec 1;29(23):2593-2602, 2004.
(7) Skytte L, May S, Petersen P; Centralization: Its prognostic value in patients with referred symptoms and sciatica Spine; 30:E293-E299, 2005.
(8) Werneke M, Hart DL:; Discriminant validity and relative precision for classifying patients with non-specific neck and back pain by anatomical pain patterns Spine; 28(2), 161-166, 2003.
(9) Werneke M, Hart DL, Resnik L, Stratford PW, Reyes A; Centralization: prevalence and effect on treatment outcomes using a standardized operational definition and measurement method. J Orthop Sports Phys Ther; 38:116-125, 2008.
(10) Young S, Aprill C, Laslett M; Correlation of clinical examination characteristics with three sources of chronic low back pain Spine; 3.460-465, 2003.
Jerry Hesch’s Reply March 26, 2010
In response to the reply from: Carol P. Dionne, PT, DPT, PhD, OCS, Cert MDT
I am in agreement with Dr Dionne’s her reply, and will elaborate in perhaps making a case for additional possibilities. Again, the outcome of the case study was very successful.
"We respectfully question if Mr. Hersh's (Hesch’s) theory of iliopsoas spasm and compression of the lateral femoral cutaneous or genito femoral cutaneous nerve has similar support in research."
The basic anatomy supports the possibility that the aforementioned nerves, which are formed within the psoas complex, can respond adversely to mechanical forces. Below are a few references on topic, though I am unaware of specific research, and have a difficult time imaging how specific research would be conducted on a live subject. However, I have a depth of empiricism. In 32 years of experiencing severe pain, I never had a single health care practitioner perform a competent evaluation of the 3 para-inguinal nerves, the ilioinguinal, iliohypogastric, and genital and femoral portions of the genitofemoral and lateral femoral cutaneous nerves. This occurred in spite of consistent subjective complaints and the use of a pain drawing, over a 32 year period. There exists a significant knowledge gap regarding peripheral neuropathies involving these nerves. Three decades post injury, when a family physician offered to perform a hernia screen, with skepticism, I obliged. This was the first time it had been offered. In my own ignorance, based on my experience of pain, I erroneously imaged a plexopathy that was non-treatable. This can be seen in Grant's Atlas of Anatomy 7th edition, fig 3-76. The hernia screen was exquisitely painful and the light bulb in my brain set off with the understanding that this was a peripheral neuropathy, hence perhaps treatable.
I developed a rudimentary 3-D pain drawing that might be helpful in diagnosing similar presentation, outlining the deep pain that cannot be visualized in traditional pain drawings. I described the internal screen, scouring the canal and spermatic cord and genital portion of genitofemoral which is proximal to the inguinal opening, as a diagnostic test, which apparently is not utilized by the medical profession. A letter from a renowned surgeon affirms the novelty of the test and is described in www.heschmanmualtherapy.com. Failing conservative care, traditional PT and Pain Management, I had a very successful triple neurectomy, though the proximal pain (within psoas to external inguinal ring) remains, albeit much less than the severe distal pain. The mechanism of injury is consistent with a stretch and compression multiple neuropathy, within the psoas and peripherally. Research is needed. In the clinical present, it is worthwhile to question presentations and look beyond a single paradigm. The results are valid in the case presentation, the theoretical construct that undergirds it can be expanded. While this case study is a successful intervention, there are others, myself included who may not be as successful, and other paradigms need to be brought to light, and researched. I welcome the opportunity to participate in research and believe it to be best accomplished with a team approach with knowledgeable educators and clinicians such as the authors of the case study. Their resources greatly exceed my own, and the need is great.
Again I submit the following: What was her hip extension prior to treatment? I can see how the treatment could enhance hip extension and lengthen a tight iliopsoas complex. The treatment was appropriate and the results stand alone. Nonetheless, I wonder if perhaps there are alternate considerations.
While I cannot specifically correlate my case with the case study, there are some overlapping consistencies that seem worthy of mention, worthy of consideration when similar presentations do not respond with traditional approaches. I believe that screening hip extension is relevant in all who present similarly.
Thank you for allowing me to pose these comments.
Sincerely,
Jerry Hesch, MHS, PT
the Hesch Method, Hesch Manual Therapy
Nerve Entrapment Syndromes of the Lower Extremity
Author: Minoo Hadjari Hollis, MD, Orthopedic Surgeon, Sound Orthopedics and Foot and Ankle Center
Coauthor(s): David E Lemay, MD, Consulting Staff, Pensacola PM&R Group, PA and Gulf Coast Orthopaedic Specialists, PA
http://emedicine.medscape.com/article/1234809-overview
Entrapment, Lateral Femoral cutaneous nerve
http://wiki.cns.org/wiki/index.php/Entrapment%2C_Lateral_Femoral_Cutaneous_Neuropathy
Handbook Of Peripheral Nerve Entrapmentsby Oscar A. Turner, Norman Taslitz (Editor), Steven Ward (Editor)Pub. Date: February 2010
http://search.barnesandnoble.com/Handbook-of-Peripheral-Nerve-Entrapments/Oscar-A-Turner/e/9780896031463
Dawson DM, Hallett M, Wilbourn AJ: “Miscellaneous uncommon syndromes of the lower extremity” 369-379 in Entrapment Neuropathies Third Edition Lippincott-Raven, Philadelphia, 1998.