Peroneal Tendonitis, Subluxation & Retinaculum Tears
The peroneal tendons are typically irritated at the lateral ankle and foot as the wrap around the lateral malleolus and traverse the retinacular tunnel. They are also irritated on the lateral and inferior portion of the cuboid where there is an indentation specific to the tendons. Not all persons are gifted with a 3rd peroneal muscle/tendon, some have a 3rd small one called the peroneus tertius. You can look that one up, good topic for a later date. There was a recent change in terminology, the peroneal muscles now named the Fibularis longus, replacing Peroneus Longus, and same first name for the Brevis and Tertius. however, it has not yet made its way into common usage. Let me guess thet the change was somewhere around 2003 and doneby the large international anatomy group, whose name escapes me! This is a very good article by Dr Sammarco. He has published extensively and is well respected. In this population my efforts would be directed at reducing the varus of the calcaneus, which in many clients is a mutable dysfunction. I utilize manual therapy, emphasizing creep (deformation over time) to restore calcaneal abduction, a key to restoring calcaneal valgus. Surprisingly, this can oftentimes be accomplished within 1-2 1-hour visits. Chances are good that these clients have not just excessive (unilateral) varus on the side with peroneal tendonitis, but they also have a Type II "Cuboid Syndrome". I place it in quotations, because the limited cuboid mobility is not necessarily painful. In working to restore calcaneal valgus/eversion, all patterns would be evaluated and treated sequentially. Please see the section on Type II Cuboid Syndrome for a review. Of course, in addition to restoring functional, normative mobility throughout the foot and ankle, in this population, treating the peroneal tendonitis would aslo be performed. This would include transverse friction massage and instruction in performing same at home, ice, compression, education in use of supports, exercise, etc. The retinaculum is like a cover, sleeve, pulley that holds the tendo in place, thus providing mechanical advantage. If it is incompetent and does not heal, or if the tendonitis is severe and does not respond to conservative measures, the followiing article becomes relevant. A more current literature search is also in order.
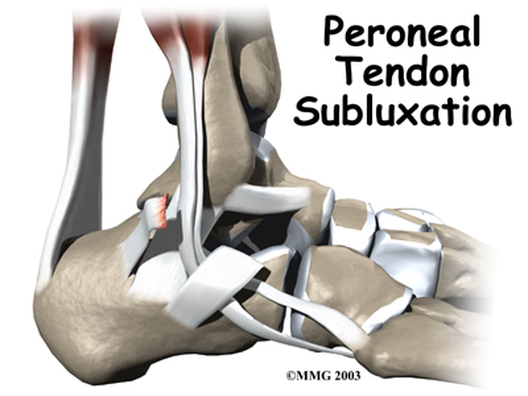
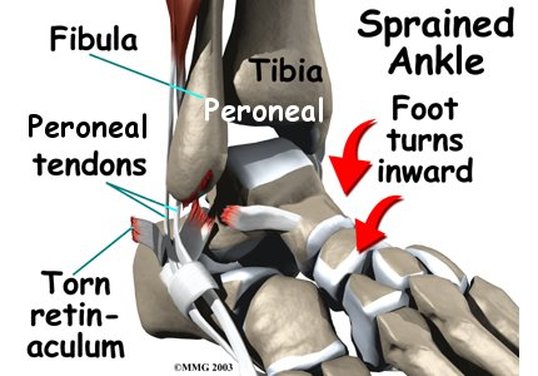
IMAGES OF PERONEAL SUBLUXATION AND RETINACULUM TEAR I must object to the term "foot turns inward", and replace with "foot turns outward"! http://www.orthogate.org/patient-education/ankle/peroneal-tendon-subluxation.html A worthwhile article on Peroneal Tendonitis. Peroneal tendonitis can lead to tendon rupture
Dividing Tendons Into Four Zones Aids in Diagnosis & Surgical Treatment
By Dave Levitan
1st on the web (May 20, 2005) (http://www.orthosupersite.com/view.asp?rID=3252)
Peroneal tendonitis and tendon ruptures can cause severe pain and immobility if left untreated, while early treatment can help patients avoid ruptures. But expect patients to require surgery when they have full ruptures or fail to respond to conservative treatment.
“Peroneal tendonitis is a common cause of lateral ankle pain. It occurs in a system of fiberosseous tunnels at the lateral aspect of the foot and ankle. Commonly it is an overuse condition that responds to conservative treatment, but if it is left untreated it can progress to a complete tendon rupture,” said G. James Sammarco, MD, of the Center for Orthopaedic Care in Cincinnati. He discussed management of peroneal tendon ruptures at the American Orthopaedic Foot and Ankle Society Specialty Day meeting at the American Academy of Orthopaedic Surgeons 72nd Annual Meeting in Washington.
1st on the web (May 20, 2005) (http://www.orthosupersite.com/view.asp?rID=3252)
Peroneal tendonitis and tendon ruptures can cause severe pain and immobility if left untreated, while early treatment can help patients avoid ruptures. But expect patients to require surgery when they have full ruptures or fail to respond to conservative treatment.
“Peroneal tendonitis is a common cause of lateral ankle pain. It occurs in a system of fiberosseous tunnels at the lateral aspect of the foot and ankle. Commonly it is an overuse condition that responds to conservative treatment, but if it is left untreated it can progress to a complete tendon rupture,” said G. James Sammarco, MD, of the Center for Orthopaedic Care in Cincinnati. He discussed management of peroneal tendon ruptures at the American Orthopaedic Foot and Ankle Society Specialty Day meeting at the American Academy of Orthopaedic Surgeons 72nd Annual Meeting in Washington.
Predisposing Peroneal Tendonitis Factors
Predisposing factors for peroneal tendonitis and rupture include varus alignment of the hindfoot and peroneal subluxation and dislocation. Participation in certain sports, including downhill skiing, skating, ballet, running and soccer creates higher risk for peroneal tendon tears. “Poorly fitting footwear, particularly ski boots and hockey skates, are often the inciting factors,” Sammarco wrote in his abstract.
If caught early, surgeons can treat peroneal tendonitis or instability conservatively with NSAIDs, immobilization and avoidance of exacerbating activities. Once secondary changes in the tendon occur, however, surgical treatment often becomes necessary. Sammarco recommended dividing the course of the tendons into four anatomic zones as follows:
1. Zone A includes the superior peroneal retinaculum and distal fibula;
2. Zone B is the inferior peroneal retinaculum at the level of the peroneal tubercle of the calcaneus;
3. Zone C involves the cuboid notch at the point the peroneus longus tendon enters the osseous groove; and
4. Zone D involves avulsion of the tendons from their insertion at the metatarsal base.
“Zone A tears usually involve the peroneus brevis, although both tendons can be involved at this level," Sammarco said. "The treatment is to ... do a side-to-side repair.” He noted the need to address nearby muscles and that sometimes accompanying muscles must be excised.
If caught early, surgeons can treat peroneal tendonitis or instability conservatively with NSAIDs, immobilization and avoidance of exacerbating activities. Once secondary changes in the tendon occur, however, surgical treatment often becomes necessary. Sammarco recommended dividing the course of the tendons into four anatomic zones as follows:
1. Zone A includes the superior peroneal retinaculum and distal fibula;
2. Zone B is the inferior peroneal retinaculum at the level of the peroneal tubercle of the calcaneus;
3. Zone C involves the cuboid notch at the point the peroneus longus tendon enters the osseous groove; and
4. Zone D involves avulsion of the tendons from their insertion at the metatarsal base.
“Zone A tears usually involve the peroneus brevis, although both tendons can be involved at this level," Sammarco said. "The treatment is to ... do a side-to-side repair.” He noted the need to address nearby muscles and that sometimes accompanying muscles must be excised.
Peroneal Tendonitis Surgical Procedures
Surgical procedures for the other zones are similar in the need for a side-to-side repair, but some aspects differ. For Zone B tears, surgeons should remove the peroneal tubercle and take care not to close the peroneal retinaculum too tight over the tendon tear. Generally speaking, surgical treatment in all zones “involves decompression of stenosis, debridement, and side-to-side repair of attritional tears and tendon repair for all cases of complete rupture,” according to the abstract.
Varus heel deformity, Sammarco noted, may require a calcaneal osteotomy, because when left untreated it can lead to further tendon problems and ankle instability. “Delayed diagnosis or chronic rupture may require [a] tendon transfer,” he wrote. “Neglected rupture may result in secondary varus foot deformity or first metatarsal elavatus.” Early and comprehensive treatment of any peroneal tendonitis or rupture is key for ensuring a good result and full recovery.
For more information:
· Sammarco GJ. Surgical technique tip I: managing complete peroneal tendon ruptures. Presented at the American Orthopaedic Foot and Ankle Society Specialty Day Meeting. Feb. 26, 2005. Washington.
Varus heel deformity, Sammarco noted, may require a calcaneal osteotomy, because when left untreated it can lead to further tendon problems and ankle instability. “Delayed diagnosis or chronic rupture may require [a] tendon transfer,” he wrote. “Neglected rupture may result in secondary varus foot deformity or first metatarsal elavatus.” Early and comprehensive treatment of any peroneal tendonitis or rupture is key for ensuring a good result and full recovery.
For more information:
· Sammarco GJ. Surgical technique tip I: managing complete peroneal tendon ruptures. Presented at the American Orthopaedic Foot and Ankle Society Specialty Day Meeting. Feb. 26, 2005. Washington.